Why are doctors concerned about dengue fever?
Every year a number of tourists catch dengue fever. Sadly, a number of these unfortunate people die of the disease.
Usually a mild or asymptomatic disease, dengue fever is, however, the cause of over 80,000 deaths each year and is a risk for over 4 billion people with 12 million reported cases annually, mainly in the Americas.
For those who develop symptoms, the experience can be traumatic. Symptoms can include severe muscle and bone pains, severe enough for the condition to be called 'breakbone fever'.
Dengue fever is caused by infection with the dengue virus, of which there are four types. Infection with one of the dengue sub-types confers lifelong immunity to that type and limited, short-term, immunity to the other types. However, subsequent infection with another dengue variant is more likely to lead to serious illness. Risk of serious illness also increases with the length of time between infections.
It has been estimated that about 5% of infections progress to serious disease with an overall mortality of 1%.
Until recently, dengue fever has been considered to be a disease of the tropics and sub-tropical regions. This is because transmission to humans is dependant upon the presence of specific mosquitoes (Aedes aegypti and Aedes albopictus) which require warm, damp conditions, with ample standing water, in order to breed. There is no human to human transmission.
The range of the mosquito vectors, and the size of the human population within that range, suggest that dengue infection is under-reported and that a large majority of infections are symptomless.
So why all the fuss?
Dengue is spreading. More specifically, the range of the insect vectors is increasing as the warm, wet conditions necessary for mosquito breeding are progressing further from the endemic equatorial regions owing to the effects of climate change. Aedes albopictus is already breeding in Southern Europe and there has been similar spread north of mosquito vectors in the United States. Estimates suggest that the disease might be endemic in the south of the UK by the middle of this century.
The overall mortality of dengue infection of 1% is similar to that seen during the recent Covid-19 pandemic but the higher caseload is likely to place a greater strain on the health services; the services that almost collapsed during the covid pandemic.
So what can be done?
Efforts to limit climate change are essential but are unlikely to have an appreciable effect upon a potential dengue pandemic. There is no specific treatment for dengue but there is a vaccine, containing attenuated virus, which has recently gained approval. The main weapon in preventing the spread of dengue is the control of mosquito numbers and breeding grounds. Clearing breeding grounds, improving sanitation, and lifting living standards is expensive, but it is an investment it would be wise to make.
Does antibiotic use during a flu infection worsen lung damage?
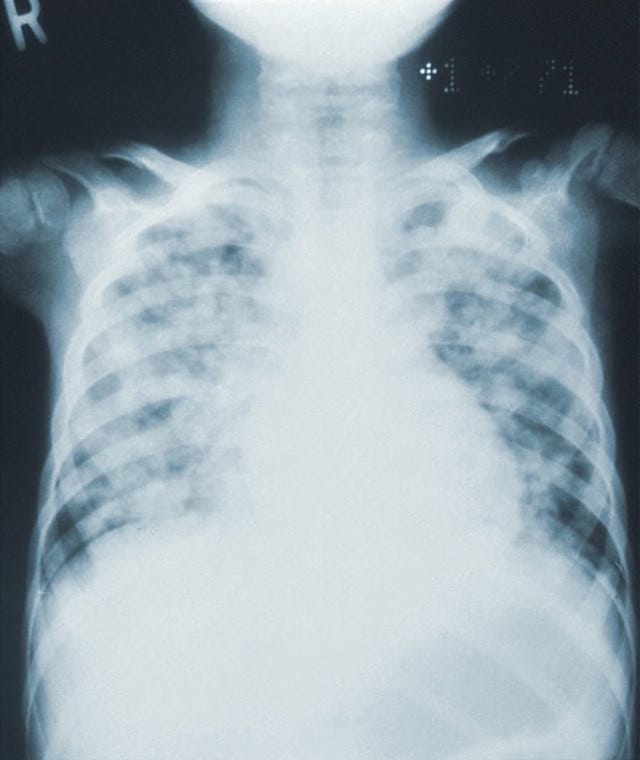
A recent study has shown that the use of antibiotic therapy during an influenza infection can damage the lung's defence against bacteria.
Antibiotic prescription for viral chest infections is unfortunately commonplace. This is partly due to clinician factors such as misdiagnosis or uncertainty, but is greatly influenced by patient pressure. Apart from the fact that such prescribing will have no beneficial effects upon the clinical course of the infection, there is also the possibility of detrimental effects such as increasing microbial antibiotic resistance, so encouraging the emergence of 'superbugs', and weakening the patient's defences to further bacterial infection. The study focused upon the latter.